What Are You Looking For?
That sudden sour taste rising in your throat after a meal or late-night snack? Many dismiss it as normal, but it could be a sign of Gastroesophageal Reflux Disease (GERD), a common yet often misunderstood digestive disorder.
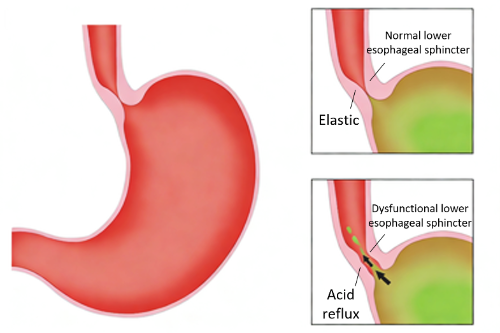
GERD occurs when stomach or duodenal contents flow back into the esophagus. Beyond classic symptoms like heartburn, acid regurgitation, and bloating, it can masquerade as chest pain, difficulty swallowing, chronic cough, laryngitis, or even asthma. This versatility makes it a master of disguise in the medical world.
If you suspect GERD, seeking professional evaluation is crucial. Diagnosis often involves a combination of tests, each assessing a different aspect of the condition.
1. Proton Pump Inhibitor (PPI) Trial
A PPI trial involves taking acid-suppressing medication (e.g., omeprazole, rabeprazole) for 4-8 weeks. Significant symptom improvement suggests GERD. However, with a specificity of only 40-50%, this test alone is not definitive. A negative response requires further investigation, and a positive one should be combined with other tests to rule out conditions like esophageal cancer or peptic ulcers.

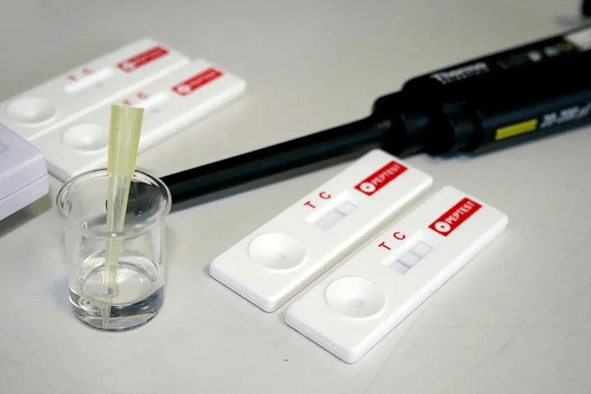
2. Saliva Pepsin Detection
This is the simplest and most non-invasive method for detecting reflux. It is ideal for children, the elderly, or patients intolerant of invasive procedures. The test analyzes a saliva sample for the presence of pepsin, a stomach enzyme that signifies reflux. It provides objective results within 15 minutes, offering a quick, accurate, and patient-friendly diagnostic clue, particularly for laryngopharyngeal reflux (LPR).
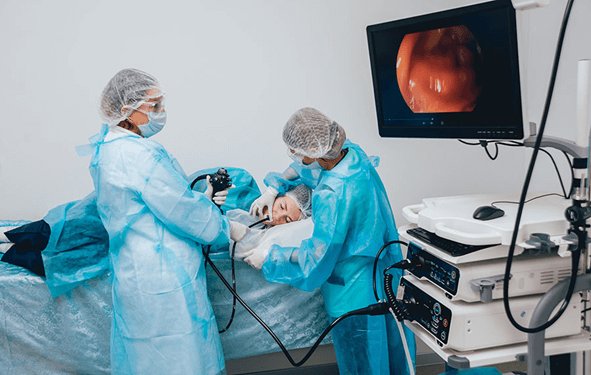
3. Upper Endoscopy (Gastroscopy)
A thin, flexible tube with a camera is passed through the mouth to examine the esophagus and stomach. This allows direct visualization of inflammation, Barrett's esophagus (a precancerous change), hiatal hernias, and other complications. It is essential for assessing tissue damage and screening for malignancies.
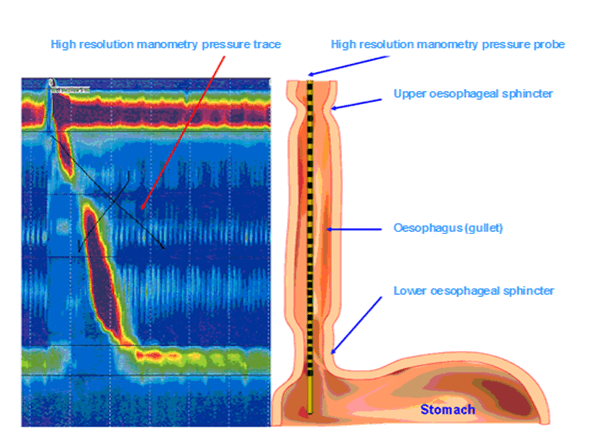
4. High-Resolution Esophageal Manometry
This test measures pressure waves in the esophagus using a thin catheter inserted through the nose. It assesses the function and coordination of esophageal muscles and the Lower Esophageal Sphincter (LES), crucial for diagnosing motility disorders and planning anti-reflux surgeries, especially in cases of hiatal hernia.
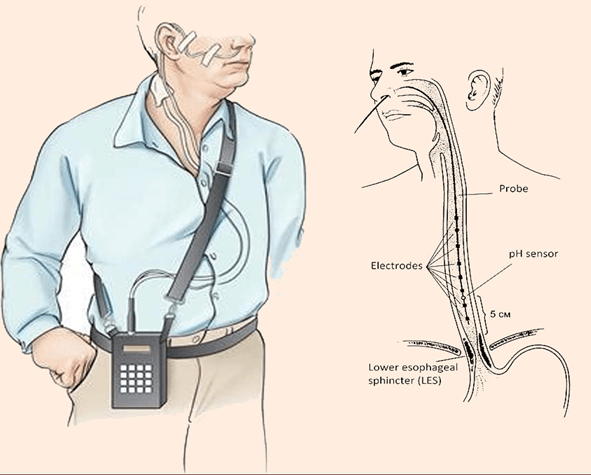
5. 24-Hour pH-Impedance Monitoring
Considered a gold standard for detecting reflux episodes, this procedure involves placing a thin monitoring probe in the esophagus for 24 hours. It measures both pH (acidity) and impedance (liquid/gas movement), identifying acid, weakly acidic, and non-acid reflux events. This data is invaluable for guiding treatment strategies and evaluating surgical outcomes.
6. Oropharyngeal pH Monitoring (e.g., Dx-pH)
Utilizing an ultra-thin probe placed in the throat, this test detects minute amounts of acidic or alkaline gas in the pharynx. It is a key tool for diagnosing Laryngopharyngeal Reflux (LPR), helping to link symptoms like hoarseness, chronic throat clearing, and cough directly to reflux.
Leave A Message